Sexually Transmitted Infections (STIs) are illnesses that are passed on via the exchange of bodily fluids during sexual activity.
Anyone who's sexually active can acquire an STI, particularly people who change partners frequently or do not use a barrier method of protection, such as a condom or dental dam, when having sex.
All STIs can be transmitted via the following routes:
- Oral sex (both giving and receiving to people of all genders)
- Penetrative vaginal sex
- Penetrative anal sex
Some STIs can be transmitted via other routes. See specific infection links for more information.
STIs are not spread by kissing, hugging, swimming in a pool, sitting on toilet seats, or sharing baths, towels, cups, plates, or cutlery.
The only way to know for sure whether you have an STI is by testing.
Regular testing is an essential part of good sexual health and ensures that you know your STI status and helps with early detection and treatment. Regular testing also reduces the likelihood that you will unknowingly pass on an STI to a partner or partners
We recommend testing:
- If you have any symptoms which could indicate an STI
- Before having unprotected sex with a new partner
- A condom splits whilst you are having sex
- A sexual partner tells you they have an STI
- You are pregnant, planning to become pregnant, or trying to get pregnant
- Every three months if you have regular unprotected sex with new or multiple partners, particularly if you have sex whilst under the influence of drugs or alcohol
- Routinely even when in a monogamous long-term relationship- it’s just good to know!
STI testing is free of charge via the NHS. If you are in the UK, visit www.nhs.uk/service-search/find-a-sexual-health-clinic/ to find your local testing clinic. Many areas will provide free online testing, whereby a sexual health screen will be sent to your home for you to complete and send off by yourself. Other areas still require you to visit a sexual health clinic in person.
Treatment for STIs varies by the infection type, and in some cases, by how advanced the STI has become. You will usually need to visit a sexual health clinic or your GP for treatment. See specific infections for more information on how specific STIs are treated.
Condoms
Condoms are the only form of contraception that also prevent against STI transmission.
Using condoms on a penis or penetrative sex toy every time you have vaginal, anal, or oral sex will significantly reduce the risk of getting or passing on STIs.
Condoms can be used for different types of sex (anal, oral, and vaginal), as well as with penetrative sex toys.
Different types of condoms available include:
- Latex, plastic, or lambskin
- Lubricated or non-Lubricated
- Spermicide-coated
- Sizes from small to king-size
- Textured (ribbed, studded, etc)
- Flavoured
- Glow-In-The-Dark
- Warming or cooling
- Extra-thin
- Extra-thick / delay (can be used to reduce sensation or delay ejaculation)
- Pleasure-shaped, twisted, extra-stimulating, fragranced, tingling etc.
Watch how to put on a condom.
All condoms with the EU and UK kite marks are equally safe; more expensive brands do not mean condoms are safer.
Femidoms/internal condoms
Femidoms, which are condoms designed to use inside a vagina and around the labia, are also available. Femidoms come in latex or latex-free condoms.
A video on how to use a femidom/internal condom.
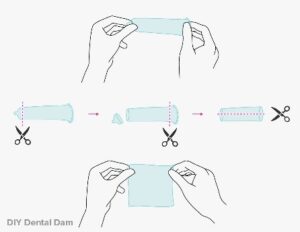
Dental dams
Dental dams are an air-tight square of latex or non-latex material designed to fit over the mouth. Dental dams act as a barrier between a mouth and a vagina or anus, and help prevent STI transmission.

A condom can also be cut open lengthwise to act as a dental-dam.
Chlamydia is the most common bacterial sexually-transmitted infection.
Chlamydia can be pass on via penetrative vaginal sex, penetrative anal sex, oral sex (to/from all genders), sharing sex toys, mutual masturbation, and from mum to baby during childbirth.
Chlamydia can also be passed to the eyes if infected genital body fluid (vaginal discharge or semen) gets into them. This most commonly happens from mum to baby during childbirth if an untreated Chlamydia infection is present.
Chlamydia can have significant long-term consequences if left untreated. Most significantly, it can lead to fertility and reproductive issues, across both genders. It can also leave to chronic pelvic inflammation and pain, or chronic testicular inflammation and pain.
Symptoms
Many people with Chlamydia (up to 70%) don't have any symptoms.
If you do develop symptoms, you may experience:
- pain when peeing
- unusual discharge from the vagina, penis, or bottom
- pain in the lower abdomen
- bleeding after sex and bleeding between periods
- pain and swelling in the testicles
Testing for and treatment for chlamydia
If visiting a clinic or ordering an at-home STI testing kit, you will be asked to provide a urine sample or to do a vaginal self-swab. In some cases, if you visit your GP or a sexual health clinic, trained staff will take a high vaginal swab. This only takes a few seconds and is not painful although you may feel slightly uncomfortable for a very short time.
Chlamydia can be treated with a course of antibiotics, and it is important that you complete the course. Staff will explain your treatment and how to avoid further infections in the future. Do tell a member of staff if you think you may be pregnant as this may affect the type of antibiotic given.
Long Term Complications
If chlamydia isn't treated, it can sometimes spread and cause potentially serious problems, including:
Pelvic inflammatory disease (PID)
Chlamydia can spread to the womb, ovaries or fallopian tubes. This can cause a condition called pelvic inflammatory disease (PID).
PID can cause several serious problems, such as:
- difficulty getting pregnant or infertility
- persistent (chronic) pelvic pain
- an increased risk of ectopic pregnancy (where a fertilised egg implants itself outside the womb)
PID is usually treated with a 2-week course of antibiotics. The risk of experiencing problems such as infertility is lower if it's treated early, so it's important to seek medical advice as soon as possible if you have symptoms of the condition.
The symptoms of PID are generally like the symptoms of chlamydia, including discomfort or pain during sex, pain during urination, and bleeding between periods and after sex.
Pregnancy complications
If you have chlamydia that's not treated while you're pregnant, there's a chance you could pass the infection on to your baby. If this happens, your baby may develop an eye infection (conjunctivitis) and lung infection (pneumonia).
If your baby has symptoms of these conditions, your midwife or GP can arrange for a test to check for chlamydia, and antibiotics can be used to treat the infection.
Untreated chlamydia in pregnancy may also increase the risk of problems such as premature labour and birth (before 37 weeks of pregnancy) or your baby being born with a low birthweight.
Inflammation of the testicles
Chlamydia can spread to the testicles and epididymis (tubes that carry sperm from the testicles), causing them to become painful and swollen. This is known as epididymitis or epididymo-orchitis. This is very rare.
The inflammation is usually treated with antibiotics. If it's not treated, there's a possibility it could affect your fertility.
Reactive arthritis
Chlamydia is the most common cause of sexually acquired reactive arthritis (SARA). This is where your joints, eyes, or urethra (the tube that passes urine out of the body) become inflamed, usually within the first few weeks after having chlamydia.
There's currently no cure for SARA, but most people get better in a few months. In the meantime, treatment with non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help relieve the symptoms.
More information
Gonorrhoea is the second most common bacterial sexually transmitted infection, with rates of Gonorrhoea currently increasing across the UK. The bacteria that cause gonorrhoea are mainly found in discharge from the penis and in vaginal fluid, though they can also be found in the anus or back of the throat.
The bacteria can infect the entrance to the womb (cervix), the tube that passes urine out of the body (urethra), the rectum and, less commonly, the throat or eyes.
Gonorrhoea can be transmitted via unprotected penetrative vaginal sex, penetrative anal sex, oral sex (to/from all genders), sharing sex toys, mutual masturbation, and from mum to baby during childbirth.
Without treatment, gonorrhoea can cause permanent blindness in a new born baby.
Symptoms
Gonorrhoea can be asymptomatic in up to 10% of men and 80% of women.
Typical symptoms of gonorrhoea include a thick green or yellow discharge from the vagina or penis, pain when peeing and, in women, bleeding between periods.
Testing and treatment
If visiting a clinic, you will be asked to provide a urine sample or to do a vaginal self-swab. In some cases, trained staff will take a high vaginal swab. This only takes a few seconds and is not painful although you may feel slightly uncomfortable for a very short time.
Gonorrhoea is be treated with a single antibiotic injection, usually administered in the buttocks. Staff will explain your treatment and how to avoid further infections in the future. Do tell a member of staff if you think you may be pregnant as this may affect the type of antibiotic given.
More information
Syphilis is mainly spread through close contact with an infected sore during unprotected vaginal, oral, or anal intercourse or other genital contact with an infected partner.
It can also be transmitted if you inject yourself with drugs and you share needles with somebody who's infected, or through blood transfusions in areas of the world where blood is not tested for Syphilis.
In the UK, Syphilis infection is relatively uncommon and was for a time considered almost obsolete. However, in recent years the numbers of cases diagnosed, particularly amongst men having sex with men (MSM).
Syphilis is especially harmful in pregnant women where infection can cause miscarriage, still birth, or foetal abnormality. A pregnant woman with infectious syphilis can pass the infection to her foetus via the placenta or during birth.
Symptoms
Many times, someone with syphilis will have no symptoms, but can still transmit the infection.
There tend to be three stages of infection:
1. Stage one - primary infection
Symptoms two to six weeks after infection can include:
- small, painless sores or ulcers that typically appear on the penis, vagina, or around the anus, but can occur in other places such as the mouth
- small skin growths (similar to genital warts) that may develop on the vulva in women or around the bottom (anus) in both men and women
2. Stage two - secondary infection
Symptoms six weeks to six months after infection can include:
- a blotchy red rash that often affects the palms of the hands or soles of the feet
- white patches in the mouth
- tiredness, headaches, joint pains, a high temperature (fever) and swollen glands in your neck, groin or armpits.
3. Stage three - tertiary infection or late syphilis
If left untreated for years, syphilis can spread to the brain or other parts of the body and cause serious long-term problems.
- Late syphilis occurs four or more years after an untreated primary infection
- Complications may occur with the heart, respiratory tract or central nervous system
Testing and treatment
The test for syphilis usually involves a blood test, or if sores are present, by removing a sample of fluid from any sores using a swab (like a cotton bud).
Some clinics offer a finger pin-prick test which indicates instantly whether Syphilis might be present.
All stages of Syphilis can be treated.
Syphilis is usually treated with either:
- an injection of antibiotics into your buttocks
- a course of antibiotics tablets if you cannot have the injection.
More information
Genital herpes (Herpes Simplex Virus 2, or HSV-2) is a viral STI that can be passed on through vaginal, anal, and oral sex as well as via skin-to-skin contact with an infected area, including via fingers.
Approximately 23% of adults in the UK carry the genital herpes virus. Many individuals with genital herpes experience outbreaks, though many others are asymptomatic.
Genital herpes is highly contagious during an outbreak- which lasts from the tingling or itching sensation which precedes the appearance of sores or blisters, until when the sores have fully scabbed over and healed.
You can still pass on genital herpes when you do not have any symptoms, though it is much less likely.
Symptoms
Many individuals with genital herpes carry the virus but do not have any symptoms.
Other individuals have one or more “outbreaks”, meaning they experience symptoms for a period, then return to having no symptoms either permanently or intermittently.
Outbreaks can involve:
- small painful blisters that burst to leave red, open sores around your genitals, anus, thighs, or bottom
- tingling, burning, or itching around your genitals
- difficulty passing urine
- pain when you pee
- unusual discharge from the vagina or penis
First outbreaks tend to be most severe. Individuals who experience recurrent herpes outbreaks often report experiencing a tingling or burning sensation around the genital region for a few days, preceding an outbreak.
Outbreaks can be triggered through illness, stress, whilst menstruating, whilst having surgery on your genital area, or when the immune system is weakened (for example, during chemotherapy). Other triggers can include exposure to UV light, friction in the genital area, tight clothing, smoking, or drinking alcohol.
Testing and treatment
Herpes is not routinely tested for as part of a routine sexual health screen.
Most healthcare professionals will only test for genital herpes if an outbreak is suspected.
If an outbreak is suspected, a healthcare professional will take a small swab to collect the fluid from one of your sores or blisters. It will be sent to a laboratory for testing.
Over time, outbreaks tend to happen less often and be less severe. Some people never have outbreaks.
Many herpes outbreaks will go away on their own.
In some cases, to decrease the length or severity of an outbreak, an individual will be prescribed:
- antiviral medicine to stop the symptoms getting worse – you need to start taking this within five days of the symptoms appearing
- cream for the pain
- Some people who have more than 6 outbreaks in a year may benefit from taking antiviral medicine for 6 to 12 months.
In the UK, you can visit your GP or a sexual health clinic if you have been diagnosed with genital herpes and need treatment for an outbreak.
If you still have outbreaks of genital herpes during this time, you may be referred to a specialist.
Genital herpes and pregnancy
Women who have herpes before pregnancy generally have healthy pregnancies and are able to have vaginal deliveries. A caesarean section might be indicated if an active outbreak is suspected.
Having genital herpes during pregnancy can also mean that your baby could develop neonatal herpes, which is a serious illness that can be fatal. Most babies recover with antiviral treatment.
The risk is highest when herpes presents for the first-time during pregnancy, and is much lower if you have had an outbreak before.
You may be offered antiviral treatment during pregnancy:
- to treat outbreaks in pregnancy
- from 36 weeks to reduce the chance of an outbreak during birth
- from diagnosis until the birth if you first get herpes after 28 weeks of pregnancy.
Genital herpes and oral herpes
Oral herpes and genital herpes are caused by two slightly different but largely similar viruses: herpes simplex 1 (HSV-1) and herpes simplex 2 (HSV-2), respectively.
Close to 70% of the population are believed to carry at least one type of the herpes virus.
Both viruses can cause sores to appear in your vulva, vagina, cervix, anus, penis, scrotum, buttocks, thighs, lips, mouth, throat, and occasionally, your eyes.
Generally, HSV-1 tends to cause oral or facial outbreaks, and HSV-2 tends to cause genital outbreaks.
HSV-1 can be transmitted to the genitals, usually through oral sex. HSV-1 outbreaks tend to be less severe, even if they present on the genitals. It is unusual for HSV-2 to be transmitted from the genital region to the oral region, though it is not impossible.
More information
HPV is the name given to a group of viruses. There are over 100 strains of HPV, four of which can cause genital warts.
HPV tends to affect the throat, mouth, or genital area. It is easily transmittable via:
- any skin-to-skin contact in the genital region
- vaginal, anal, or oral sex
- sharing sex toys
- mutual masturbation
Symptoms
Many people with HPV are unaware they are infected as they have no symptoms.
When genital warts do present, it is called an outbreak. Outbreaks can include:
- painless lumps or growths to appear around your vagina, penis, or anus
- itching from your genitals or anus
- bleeding from your genitals or anus
- a lasting change in your urinary flow (eg, your wee goes to the side)
Testing and treatment
HPV is not routinely tested for, even as part of a routine sexual health screen.
If warts are suspected, a visual exam will take place, either at your GP or at a sexual health clinic. This exam may include the use of a magnifying lens. Your healthcare provider might need to look inside your vagina, anus, or urethra.
Any warts using one of the following methods:
- self-applied cream or liquid
- healthcare provider-applied cream or liquid
- surgery to cut, burn, of laser off the warts
- freezing
It can take several weeks or months for treatment to fully eradicate all warts.
Genital warts might return. However, new research indicates that it is possible for your body to eventually clear itself of the virus, so no future outbreaks will happen unless a new infection is acquired.
Other strains of HPV
Other strains of HPV, considered “high-risk” types, can cause abnormal changes in the body’s cells that can eventually turn into certain cancers including:
- cervical cancer
- anal cancer
- cancer of the penis
- vulval cancer
- vaginal cancer
- certain types of head and neck cancer
In the UK, HPV testing is included as part of routine cervical screening for people with a cervix aged 25-64. During a cervical screen, a small sample of cells is taken from the cervix by a trained healthcare provider.
Routine cervical screening is important to ensure that any abnormal cell development is caught early, and can be treated.
More information on the UK Cervical Screening programme.
HPV vaccination
Young people in the UK are offered an HPV vaccine between the ages of 12 and 13. The vaccine is given in two doses, spaced six months to two years apart. The vaccine protects against most strains of HPV that cause genital warts, as well as the strains of HPV responsible for 70 per cent of cervical cancer cases and some cancers of the anus, vulva, vagina, and penis.
Men having sex with men (MSM), and some trans-women and trans-men can also get the vaccine free of charge at sexual health clinics, up to the age of 45.
More information
Pubic lice (sometimes called crabs) are tiny insects that live on coarse human body hair, such as pubic hair.
As well as being found in pubic hair, the lice are also sometimes found in:
- underarm and leg hair
- hair on the chest, abdomen and back
- facial hair, such as beards and moustaches
Pubic lice don't live in scalp hair.
Pubic lice are spread through close bodily contact, especially sexual contact. Less commonly, they can also be passed on through sharing clothes, towels, and bedding.
Symptoms
Symptoms include:
- itching in the affected areas, especially at night
- inflammation and irritation caused by scratching
- black powder in your underwear
- blue spots or small spots of blood on your skin, such as on your thighs or lower abdomen
Testing and treatment
Your GP or a sexual health clinic will perform a visual exam to determine whether you have pubic lice. They might need to use a magnifying class.
Treatment can include an insecticide cream, lotion, or shampoo and usually needs to be repeated after 7 days. Persistent public lice might require more than one form of treatment, as some lice have become resistant to certain treatments.
If you suspect you have public lice, you can also visit a pharmacy to see if they can offer advice and treatment over the counter.
More information
We have included the most common STIs.
For more information about STIs in general, as well as specific STIs not included, see:
Scabies
Scabies is a common and highly contagious skin condition, that is passed on via skin-to-skin contact (including, but not limited to, sexual contact).
People who live or work together closely, such as in halls of residence or nursing homes, are more at risk.
Symptoms include intense itching, and a raised rash or spots that often present in a linear pattern with a red dot at one end. The rash is often first spotted on the hands, in between the fingers. The rash quickly spreads across the whole body.
If you suspect you have scabies, visit your local pharmacist who will advise you on treatment. Everyone in your home or living quarters will need to be treated at the same time, as should anyone you have had sexual contact with in the previous 8 weeks.
More information on scabies.
Bacterial Vaginosis (BV)
BV is a common cause unusual vaginal discharge that is at times accompanied by a strong fishy smell, particularly following sex.
BV is often mistaken for an STI, though it is not. BV is caused by an imbalance in the bacteria in your vagina. Sometimes BV “just happens”, and other times it is caused by:
- a new sexual partner, or multiple sexual partners
- the IUD contraceptive device
- using perfumed or fragranced products around your vagina
Having BV can make you more susceptible to acquiring an STI, because your vagina becomes less acidic and therefore less able to naturally defend itself against infection.
Some treatment for BV can be purchased over the counter in the UK. Other times you will need to visit your GP or a sexual health clinic for antibiotic tablets or creams. Recurrent or treatment-resistant BV can require longer treatment.
More information on BV.
Thrush (candidiasis or yeast infection)
Thrush is a yeast infection that can infect your vagina. It is caused by the candida species of fungus, which normally lives happily inside the vagina, and does not cause any problems, because it is kept under control by healthy bacteria.
However, changes to the balance of bacteria can create conditions in which the fungus can grow, which can cause:
- white discharge (like cottage cheese), which does not usually smell
- itching and irritation around the vagina and vulva
- soreness and stinging during sex or when you pee
- redness
Like BV, thrush is often mistaken for an STI, even though it is not. However, because thrush can be passed back and forth between partners, both partners should treat for thrush at the same time to avoid recurrent infections.
Treatment for thrush can be bought over the counter in most pharmacies. Thrush treatment usually involves itching relief as well as an anti-fungal treatment.
More information about thrush.
Monkeypox
Monkeypox is a virus that was first identified in colonies of monkeys kept for research. Cases in many countries worldwide are currently rising.
While not classed as a sexually transmitted infection (STI) it is transmitted through close, personal and skin-to-skin contact.
- Direct contact with monkeypox rash, scabs, or body fluids from a person with monkeypox.
- Touching objects, fabrics (clothing, bedding, or towels), and surfaces that have been used by someone with monkeypox.
- Contact with respiratory secretions.
This direct contact can happen during intimate contact, including:
- Oral, anal, and vaginal sex or touching the genitals (penis, testicles, labia, and vagina) or anus (of a person with monkeypox.
- Hugging, massage, and kissing.
- Prolonged face-to-face contact.
- Touching fabrics and objects during sex that were used by a person with monkeypox and that have not been disinfected, such as bedding, towels, fetish gear, and sex toys.
These methods of transmission mean that barrier methods are insufficient for protecting against monkeypox and all intimate contact needs to be avoided until the rash has healed and symptoms have resolved.
Symptoms
Monkeypox symptoms usually start within three weeks of exposure to the virus. If someone has flu-like symptoms, they will usually develop a rash one to four days later. You may get a rash that may be located on or near the genitals (penis, testicles, labia, and vagina) or anus, or could be on other areas like the hands, feet, chest, face, or mouth. The rash will go through several stages, including scabs, before healing and can initially look like pimples or blisters and may be painful or itchy.
Other symptoms of monkeypox can include:
- Fever
- Chills
- Swollen lymph nodes
- Exhaustion
- Muscle aches and backache
- Headache
- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
You may experience all or only a few symptoms
- Sometimes, people have flu-like symptoms before the rash.
- Some people get a rash first, followed by other symptoms.
- Others only experience a rash.
Monkeypox can be spread from the time symptoms start until the rash has healed, all scabs have fallen off, and a fresh layer of skin has formed. The illness typically lasts two to four weeks.
